From bed-sized iron lungs to portable, computer-controlled systems, the ventilators used to treat life-threatening respiratory diseases—and so much in demand today—have had a “remarkable journey.”
It was painful to watch. At the height of the epidemic, hundreds of patients arrived at hospitals, smothering or drowning in their own secretions. The demand for ventilators far exceeded their supply. Sound familiar?
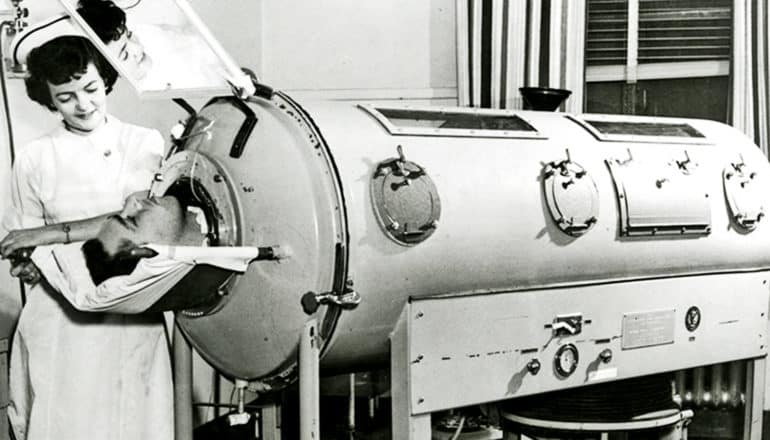
In 1931, the epidemic was polio. The victims were mostly small children, many with lungs paralyzed by the disease. And the ventilator, invented just three years before at Harvard Medical School, was the “iron lung”—initially a rectangular metal box in which individual patients were placed with only their heads protruding.
Air pumps from two vacuum cleaners changed the pressure inside the box, pulling air in and out of the lungs.
Refined versions of iron lungs became the mainstay in treating polio victims during the next three decades. In 1939, the National Foundation for Infantile Paralysis began mass distribution of iron lungs, which cost about $1,500 each—then the average price of a home.
Eugene Farley neared completion of his medical degree at the University of Rochester during one of the last major polio outbreaks. Patients in iron lungs filled two wings of Strong Hospital. “Helping care for these patients paid for my senior year of medical school,” Farley says.
Even in the 1950s, however, the shortage of iron lungs was so acute that tubes had to be inserted in some patients through the mouth or by tracheotomy to force air into their lungs. This measure, previously used only in the operating room, also saved lives.
Back to normal breathing
Modern mechanical ventilators—whose short supply is now at the center of a national debate about the nation’s preparedness for the COVID-19 pandemic—bear little resemblance to the cumbersome iron lungs that saved thousands of lives before the development of a polio vaccine in the mid-1950s.
The modern devices—used to assist or actually substitute for a patient’s normal breathing in a wide range of clinical scenarios—are smaller, more portable, and are electronically controlled by microchips to exactly adapt air flow and pressure to an individual patient’s needs. They are the result of more than three centuries of experimentation and design.
And the Lord God formed man of the dust of the ground and breathed into his nostrils the breath of life. (Genesis 2:7)
And he [Elisha] went up, and lay upon the child, and put his mouth upon his mouth and the flesh of the child waxed warm. (II Kings 4:34)
As the two Old Testament passages above suggest, humans have known how to use mouth-to-mouth resuscitation to force air into stricken lungs—a form of “positive pressure” ventilation—at least as early as Biblical times.
However, Robert Hooke, the scientist who coined the word “cell,” may have been the first to experiment with mechanical ventilation. In the 17th century, he demonstrated that mechanical ventilation can help do the work of damaged lungs by using a bellows to blow air into the injured lungs of a dog.
During the 1800s and early 1900s, negative-pressure ventilators predominated, mimicking the normal breathing process. The systems worked because when we expand our rib cage and chest cavity, it decreases pressure in the cavity, causing the lungs to expand as well. That causes air inside the lungs to decrease—creating negative pressure relative to the atmosphere—which results in air flowing into the lungs through inhalation.
For example, in 1838 Scottish physician John Dalziel described a full-body type “tank ventilator.” It consisted of an airtight box in which a patient sat, with only the head protruding. Manually pumping air into and out of the box established negative pressure.
This led to the negative pressure “iron lungs” and eventually smaller, more portable devices used to treat polio victims.
For example, Rochester Review in June 1959 (page 26) reported that John H. McKeehan, a mechanical engineering alumnus living in Syracuse, had “taken it upon himself to see that the chest shell respirators, in which two neighbors who have been stricken with polio must live, are functioning properly night and day.”
McKeehan greased the devices and checked their batteries every month, and twice a year took the artificial lungs completely apart and rebuilt them. “‘This is a pretty tense job; it could be disastrous if I accidentally stripped a screw, for instance,'” he explained. To do this job he searched out and studied a service manual for the respirators “which are a compact version of the familiar iron lung.”
At the time, the devices were usually referred to as “respirators”—a term now used for protective face masks.
From past to present
In the 1960s there was a movement away from negative-pressure ventilators in favor of positive-pressure devices that force air into a patient’s lungs, either noninvasively with nose or face masks for less severe breathing problems or by invasively inserting tubes in a patient’s airway.
Robert Kacmarek, director of respiratory care at Massachusetts General Hospital and a professor of anesthesiology at Harvard Medical School, describes this “remarkable journey” in a 2011 paper.
“In just 50 short years we have gone from relatively crude, totally mechanical devices that could provide only machine-triggered volume ventilation to highly evolved microprocessor-controlled systems capable of any form of ventilatory support imaginable,” he writes.
These systems include:
- CPAP (Continuous Positive Airway Pressure) machines, which deliver slightly pressurized air through a small nose mask. They are commonly used to treat sleep apnea but are also used for patients with pulmonary vascular disease and in Neonatal Intensive Care Units (NICU) for infants with breathing problems, such as respiratory distress syndrome. They have not been recommended for COVID-19 because of studies suggesting such devices can pump viruses into the air, potentially increasing the spread of a contagious disease.
- BiPAP (Bilevel Positive Air Pressure) machines that raise the pressure to push air during inhalation, then lower it to allow exhalation. They are used to treat obstructive sleep apnea, chronic obstructive pulmonary disorder, pneumonia, asthma flare-up, poor breathing after an operation, and neurological disease that disturbs breathing. The settings on these machines may allow them to be adjusted to treat COVID-19 patients.
- Invasive positive-pressure ventilator machines used for patients who cannot breathe on their own or suffer from severe respiratory disease. Air is delivered through tubes inserted in a patient’s airway. These machines, used in intensive care units and as anesthesia ventilators in operating rooms, are needed for treating severe cases of COVID-19.
Elizabeth Palermo, an assistant professor of clinical nursing and specialty director of the Adult-Gerontology Acute Care Nurse Practitioner Program at the School of Nursing, is grateful for the positive impact the machines have had.
For example, the microprocessors in modern ventilators “not only determine the pressure inside the lungs,” but also adjust the timing, flow, and delivery of pressure and air to the lungs so that they are “customized for the patient’s condition and help the patient work better with the vent,” she says.
“Ventilators used to take up a great deal of valuable space in a room. Now, they are smaller, something every nurse in a crowded patient room appreciates,” says Palermo. They also have more readable displays to easily attend to the patient’s performance on the vent.
“When transporting patients on ventilators from ICUs to diagnostic tests or the operating room, we used to have to manually breathe for them using a bag-like device,” she says. “Depending on how long the trip was, this could be exhausting for the nurse and not very comfortable for the patient. Now, ventilators are much more portable, so patients can stay on a ventilator as they are transported across the hospital.”
Ventilation technology takes a team
With the advances in technology have also come an increased recognition and understanding of the risks involved in mechanical ventilation, Palermo adds.
“We have learned that too much pressure delivered by the ventilator can further injure the lungs, above and beyond the damage done by the disease itself,” she says.
“Patients on ventilators are prone to pneumonia, skin ulcers, and weakness, among other problems. We have learned that heavily sedating patients on ventilators makes it harder for them to become free of the ventilator when their lungs have healed. Our recognition of these problems and the efforts made to prevent them are probably the most important advances I have seen.”
She cautions that “ventilators do not cure disease. They allow the health care team to provide supportive care and ensure adequate oxygen delivery while treatments, such as antibiotics for pneumonia, take effect, allowing lungs injured by something like coronavirus to rest and heal.”
Moreover, using a ventilator to manage a patient’s respiratory problem is not as simple as “let’s buy more ventilators,” Palermo says. It requires a team effort involving:
- A knowledgeable physician, nurse practitioner, and/or physician assistant “to determine the need for ventilation and if it is consistent with the patient’s wishes or advance directives.”
- A competent respiratory therapist who understands the technical aspects of the ventilator machine and can adjust the pressure, oxygen, and alarms to ensure the ventilator helps the patient without causing injury.
- A competent nurse at the bedside, educated in caring for patients on ventilators, who can closely monitor a patient’s condition, respond to alarms, and use evidence-based practice to prevent injury or complications.
“The critically ill patient with respiratory failure due to COVID-19 needs a knowledgeable interdisciplinary team that communicates closely with each other to coordinate that patient’s care.”
Source: University of Rochester
The post The history of ventilators is a ‘remarkable journey’ appeared first on Futurity.
from Futurity https://ift.tt/2JXr00u
No comments:
Post a Comment