
New research provides insights into the earliest stages of Angelman syndrome.
The new study also shows how human cerebral organoids can help shed light on genetic disorders that affect human development.
Angelman syndrome is a genetic disorder associated with delayed development, intellectual disability, speech impairment, and problems with movement.
Scientists have done a great deal of research on Angelman syndrome, primarily involving laboratory studies of mice and natural history studies of humans.
However, while researchers have established that the complex disorder is tied to the behavior of a gene called UBE3A, and strong evidence in mice has shown that prenatal time periods may be important in disease development, researchers had yet to find a way of monitoring the earliest stages of the disease in human neural cells.
“Obviously we cannot do studies on developing humans, so we wanted to know whether it was possible to study the molecular dynamics around UBE3A using cerebral organoids,” says Albert Keung, assistant professor of chemical and biomolecular engineering at North Carolina State University and corresponding author of the paper in Stem Cell Reports.
“When is the gene turned on? How do drugs affect gene and neuronal functions? Does the gene behave differently in different types of cells? These are complex questions, but we found that you can learn a lot through the cerebral organoid model.”
“Organoid models aren’t new. But they may be more powerful tools than we previously anticipated.”
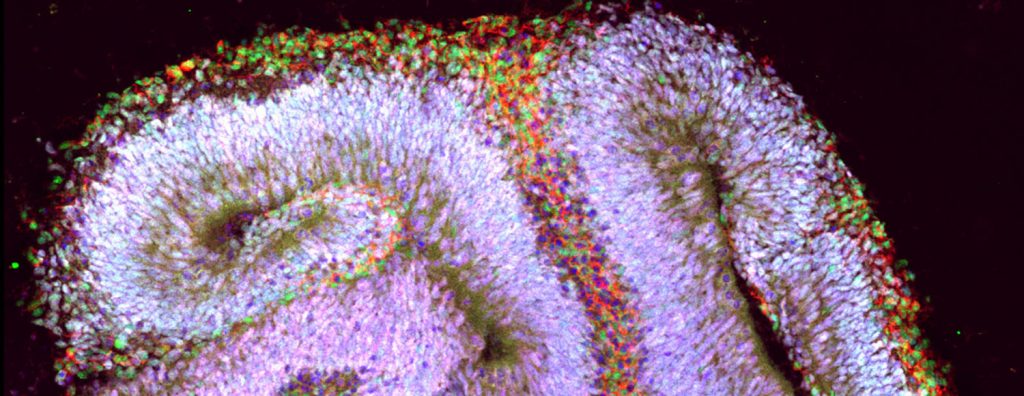
Human cerebral organoids are millimeter-sized tissues comprised of the cell types typically found in the different regions of the brain. They are made by culturing stem cells. For this study, the researchers monitored the behavior of the organoids for 17 weeks after culturing the cells.
For example, the researchers mapped when UBE3A turned off or on in different types of cells and at different stages of neurodevelopment—as well as where in each cell the gene was active. This can shed light on things such as the extent to which UBE3A might be regulating the activity of other genes, and when the delivery of therapeutic treatments may be most effective.
One of the things the researchers discovered is that UBE3A appears to be playing an important role in the development of brain tissue earlier than anyone knew—potentially even within three weeks of culturing the organoids.
“We had the ability to see how UBE3A’s behavior changed over time in the organoid,” says PhD student Dilara Sen, the paper’s first author. “We were also able to see how different drugs affected the gene’s behavior—and how those changes affected the function of neurons in the organoid.”
“This is fundamental, proof-of-concept work,” Keung says. “But hopefully it demonstrates how the cerebral organoid model can facilitate the development of therapeutic strategies for people with Angelman syndrome. We believe the model can do this by advancing our understanding of the disease, which can inform research into possible treatments. We also believe that this model could be used to screen drugs that are candidates for therapeutic interventions. Organoid models aren’t new. But they may be more powerful tools than we previously anticipated.”
The National Science Foundation, the National Institutes of Health, a Simons Foundation SFARI Explorers Grant, and a fellowship from the American Association of University Women funded the work.
Source: NC State
The post Lab-made brains shed light on Angelman syndrome appeared first on Futurity.
from Futurity https://ift.tt/33B3dNs
No comments:
Post a Comment